New findings show that stool transplants help ease symptoms and heal the colons of patients with tough-to-treat ulcerative colitis.
A study conducted by Australian scientists says that these findings could open doors in stool transplants for widespread uses. Transferring fecal matter from healthy donors to colitis patients alters the makeup of gut bacteria, which in turn puts a stop to one of the driving factors behind ulcerative colitis.
Dr. Sudarshan Paramsothy, study author and gastroenterologist at University of New South Wales, says that, “We were not completely surprised by the study findings, as . . . smaller studies along with unpublished experience suggested repeated fecal microbiota transplantation may be an effective treatment for ulcerative colitis.”
This study shows that [stool transplant] is a very promising therapeutic option for ulcerative colitis patients.
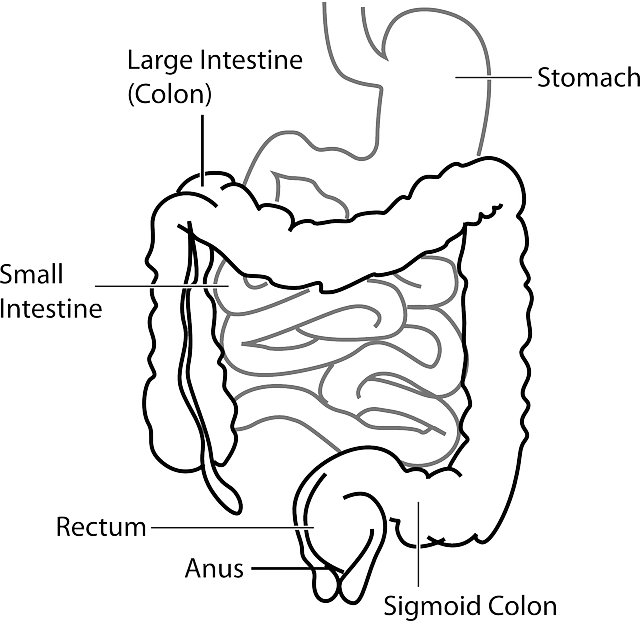
Some 700,000 Americans suffer from ulcerative colitis, which is a chronic disease doctors believe come from an abnormal immune system response. The Crohn’s and Colitis Foundation of America states that the disease causes the lining of the colon to become inflamed and develop tiny, open ulcers. Symptoms include bloody stools, diarrhea and abdominal pain.
Stool transplants, which even doctors and scientists admit has a disgusting sound to it, is currently only used for certain gastrointestinal infections which can be life-threatening.
Paramsothy and his team analyzed 81 ulcerative colitis patients across three Australian states whose diseases had not been responding to standard treatments like steroids or anti-inflammatories. The patients were randomly divided into two groups, with 41 of them receiving repeated fecal transplants in eight weeks and the others receiving a placebo.
The fecal matter used in the transplants were taken from at least three donors per patient to make sure that the results would not be affected by a single donor’s gut bacteria. Multiple donations were needed for the 40 infusions required for each patient undergoing the transplants, who personally did their infusions after the first treatment. Donor stool was filtered and homogenized, then frozen for storage. It was infused as a “slurry” directly into the rectum.
“There is a risk of infection transmission whenever a biological product is [used],” Paramsothy says. “But this can be minimized by comprehensive screening of history [and] stool and blood testing for known pathogens.”
After eight weeks, 27% of the stool transplant recipients reported no ulcerative colitis symptoms. Endoscopic examination by doctors proved that the lining of the colon in these patients had healed or significantly improved. In the placebo group, only 8% of the patients achieved the same.
Upon initial survey of patients who had undergone the transplant, but without the colon inspection, 44% of the stool transplant patients said they felt no symptoms, compared to 20% in the placebo group.
While this is impressive, Paramsothy and his team agree that more research is needed to establish the long-term effects stool transplants might have on ulcerative colitis patients.
The study is set to be present at Digestive Disease Week in San Diego. Results are considered preliminary until they have been published in a peer-reviewed journal.